
Why Perinatal Mental Health Matters to Every Family
Perinatal mental health refers to your emotional, social, and mental well-being during pregnancy and up to one year after childbirth. Here's what you need to know:
- What it is: Mental health conditions that occur during pregnancy or the first 12 months postpartum
- How common: Affects 10-20% of pregnant women and new parents (up to 27% in some studies)
- Who it affects: All parents, including birthing and non-birthing partners
- Why it matters: Untreated conditions can impact maternal health, infant development, and family well-being
- The good news: These conditions are treatable with proper support and evidence-based care
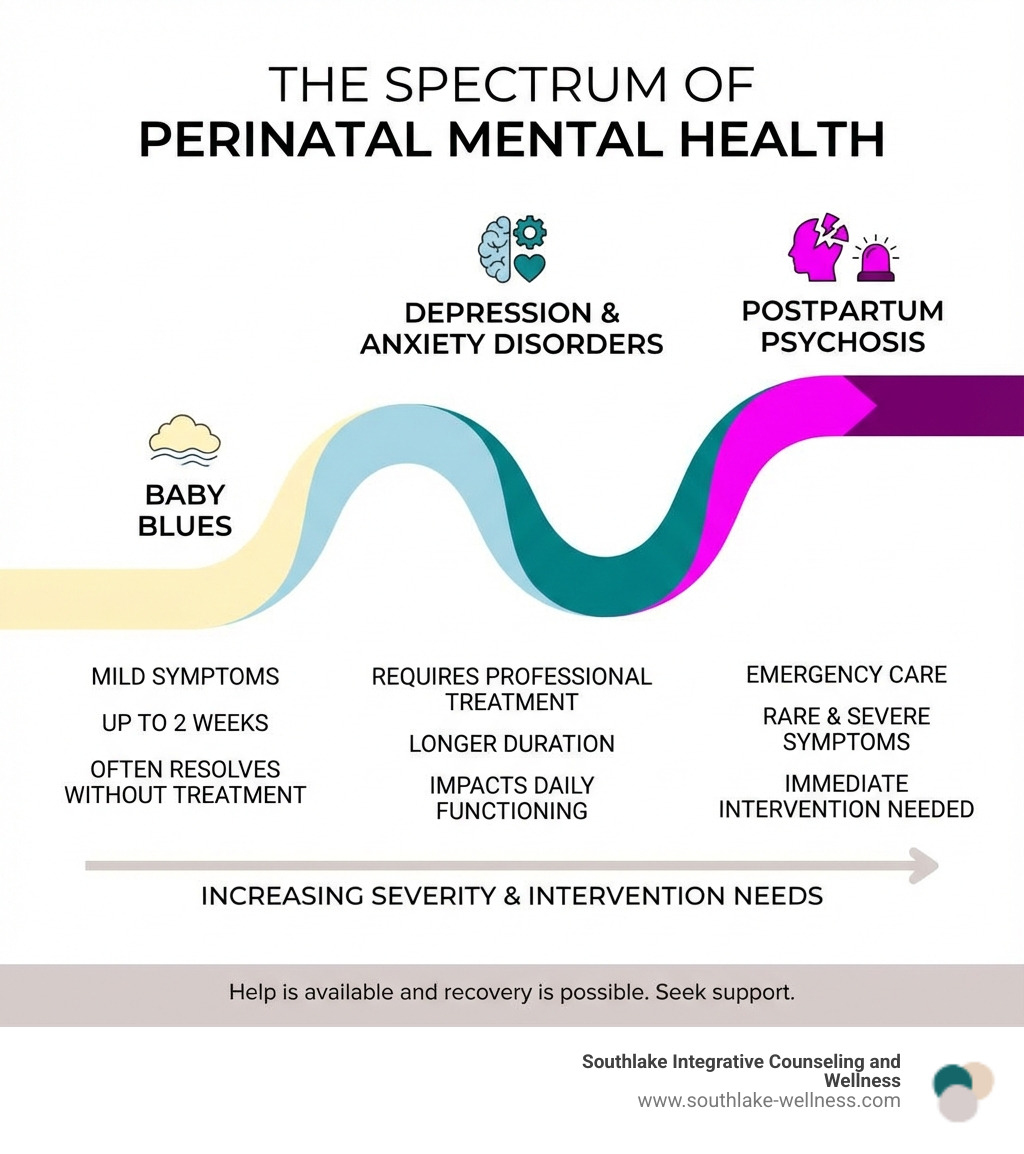
Pregnancy and new parenthood bring massive life changes. While many people experience mild mood shifts called "baby blues" that resolve within two weeks, perinatal mood and anxiety disorders are more serious conditions that last longer and require professional treatment.
These disorders aren't a sign of weakness or failure. Affecting countless families each year, perinatal mental health challenges are among the most common complications of pregnancy and postpartum. The most important thing to know is that help is available and recovery is possible.
Understanding Perinatal mental health and accessing the right support can transform your experience of this life transition.
Understanding Perinatal Mental Health: More Than Just "Baby Blues"
Parenthood is often depicted as joyful, but it's also a period of profound physical, emotional, and social adjustment. During this life stage, perinatal mental health comes into sharp focus.
What is Perinatal Mental Health?
Perinatal mental health encompasses the emotional, social, and mental well-being of individuals from pregnancy through the first year after childbirth. This period is a time of immense change, hormonal shifts, and new responsibilities, acknowledging that mental well-being is deeply intertwined with physical and social circumstances.
Perinatal mental health affects all parents, including non-birthing partners dealing with their own adjustments. Experiencing mental health challenges is never a sign of weakness or a reflection of your love for your baby. It's a common medical condition that deserves understanding and treatment.
"Baby Blues" vs. Perinatal Mood and Anxiety Disorders (PMADs)
It's vital to differentiate between the transient "baby blues" and more severe Perinatal Mood and Anxiety Disorders (PMADs). Many new parents mistakenly believe their persistent struggles are just the "baby blues," delaying much-needed help.
| Feature | "Baby Blues" | Perinatal Mood and Anxiety Disorders (PMADs) |
|---|---|---|
| Symptoms | Mild sadness, weepiness, mood swings, irritability, anxiety, feeling overwhelmed. | Severe and persistent sadness, anxiety, hopelessness, guilt, worthlessness, panic attacks, obsessive thoughts, extreme fatigue, difficulty sleeping or eating, thoughts of self-harm or harming the baby. |
| Duration | Typically begins within a few days after birth and lasts up to two weeks. | Lasts longer than two weeks, often persisting for months or even a year or more without intervention. |
| Severity | Mild, does not significantly interfere with daily functioning or bonding. | Moderate to severe, significantly impacts daily functioning, relationships, and the ability to care for oneself and the baby. |
| Intervention | Usually resolves on its own with rest, support, and self-care. | Requires professional diagnosis and treatment (therapy, medication, or a combination) to improve. |
While "baby blues" are a common and normal part of the postpartum adjustment for many, affecting up to 80% of new mothers, PMADs are more serious. Perinatal mood and anxiety disorders are among the most common complications that occur in pregnancy or in the first 12 months after delivery, affecting between 10 and 20 percent of pregnant women and new mothers, and up to 27% of new and expectant mums in some studies.
The Importance of Seeking Help: Risks of Untreated Conditions
Ignoring or downplaying perinatal mental health challenges can have significant and lasting consequences for everyone involved. Untreated conditions are not just difficult for the individual experiencing them; they can ripple through the entire family system.
- Maternal Health Risks: Prolonged depression, increased risk of chronic mental health conditions, and in severe cases, thoughts of self-harm or suicide. Untreated mental illness during pregnancy can lead to low infant birth weight and preterm delivery.
- Infant Health Risks: Research shows that untreated maternal mental illness can impact infant cognitive development, leading to increased risk of childhood emotional and behavioral problems. The American Academy of Pediatrics highlights that untreated perinatal mental illness is an Adverse Childhood Experience (ACE) with lifelong impacts on a child’s development.
- Impaired Parent-Infant Bonding: Difficulty bonding with the baby is a common symptom of PMADs. This can affect the parent's ability to respond to the baby's needs, potentially impacting the child's secure attachment and overall development.
- Adverse Childhood Experiences (ACEs): Untreated parental mental health issues can contribute to a child’s exposure to ACEs, which are traumatic events that can have a lasting negative impact on health and well-being.
- Family and Relationship Conflict: The stress and emotional toll of untreated PMADs can strain relationships with partners, other children, and extended family, leading to conflict and dissatisfaction.
We understand that reaching out for help can feel daunting, especially when dealing with the stigma surrounding mental health. However, seeking help is a courageous step and a testament to your strength. At Southlake Integrative Counseling and Wellness, we offer support to help you heal emotional trauma and develop healthier coping mechanisms. You can learn more about how we help individuals overcome emotional challenges by visiting our page on healing emotional trauma.
Recognizing the Signs: Common Perinatal Mental Health Conditions
Understanding perinatal mental health begins with recognizing that PMADs are a spectrum of disorders, each with distinct symptoms.
Common Signs and Symptoms to Watch For
It can be hard to distinguish "normal" new parent exhaustion from something more. Here are common signs that may indicate a perinatal mental health condition:

- Persistent Sadness or Crying: Feeling sad, empty, or overwhelmed most of the day, nearly every day, with frequent, uncontrollable crying.
- Excessive Worry or Anxiety: Constant, intrusive worries about the baby's well-being or your parenting ability, which can manifest as panic attacks or restlessness.
- Irritability or Anger: Unusual levels of irritability, anger, or rage directed at your partner, baby, or yourself.
- Feelings of Guilt or Worthlessness: Believing you are a bad parent, feeling inadequate, or experiencing profound guilt about your feelings or circumstances.
- Loss of Interest in Hobbies: A noticeable decrease in pleasure or interest in activities you once enjoyed, including spending time with loved ones.
- Difficulty Bonding with the Baby: Feeling detached, indifferent, or even resentful towards your baby. This can also include a lack of interest in caring for the baby.
- Scary or Intrusive Thoughts: Unwanted, repetitive, and disturbing thoughts or images about harm coming to the baby or yourself. These thoughts are terrifying but rarely acted upon. Books like "Good Moms Have Scary Thoughts" can provide helpful guidance and reassurance.
- Changes in Sleep and Appetite: Significant changes, such as insomnia even when the baby is sleeping, sleeping too much, or a loss of appetite or overeating.
- Fatigue and Low Energy: Profound exhaustion that doesn't improve with rest, making it hard to perform daily tasks.
- Physical Aches and Pains: Unexplained physical symptoms like headaches, stomach problems, or muscle pain that don't respond to treatment.
If you or a loved one notice several of these symptoms lasting for more than two weeks, it's crucial to seek professional help.
Types of Perinatal Mood and Anxiety Disorders
Perinatal mental health challenges can take several forms, each requiring specific understanding and care:
- Perinatal Depression (PND/PPD): This includes depression during pregnancy and after childbirth. Symptoms range from mild to severe and include persistent sadness, hopelessness, and difficulty bonding. About 12% of birthing parents experience it.
- Perinatal Anxiety Disorders: Characterized by excessive, uncontrollable worry that interferes with daily life, often exacerbated by the stresses of parenthood.
- Perinatal Obsessive-Compulsive Disorder (OCD): Involves intrusive, unwanted thoughts (obsessions) often related to harm coming to the baby, followed by repetitive behaviors or mental acts (compulsions) aimed at reducing anxiety or preventing perceived harm.
- Postpartum Post-Traumatic Stress Disorder (PTSD): Can develop after a traumatic birth experience, medical complications, or other events during the perinatal period. Symptoms include flashbacks, nightmares, avoidance of reminders, and heightened arousal.
- Postpartum Psychosis: A rare but severe psychiatric emergency, typically starting within weeks of birth. Symptoms include delusions, hallucinations, rapid mood swings, and confusion, requiring immediate medical attention.
At Southlake Integrative Counseling and Wellness, we use evidence-based approaches like Cognitive Behavioral Therapy (CBT) to address anxiety and other PMADs. To learn more about how CBT can help, explore our comprehensive guide to Anxiety CBT.
Key Risk Factors You Should Be Aware Of
While perinatal mental health conditions can affect anyone, certain factors can increase an individual's vulnerability:
- Personal or Family History of Mental Illness: A personal or family history of depression, anxiety, or other mental health conditions significantly increases your risk.
- Previous PMAD: If you've experienced a PMAD during a previous pregnancy or postpartum period, you are more likely to experience it again.
- Lack of Social Support: Feeling isolated, having limited help from family or friends, or lacking a supportive partner can heighten vulnerability.
- Relationship Stress: Conflict with a partner, dissatisfaction in a relationship, or domestic challenges can contribute to mental health struggles.
- Traumatic Birth Experience: A difficult or traumatic birth can lead to PTSD or exacerbate other mental health conditions.
- Hormonal Fluctuations: The dramatic hormonal shifts during pregnancy and postpartum can impact brain chemistry and mood regulation.
- Life Stressors: Major life events like financial difficulties, job loss, housing instability, or recent bereavement can increase risk.
- Complications During Pregnancy or Postpartum: Medical complications for the birthing parent or baby can add significant stress and anxiety.
Understanding these risk factors allows for proactive monitoring and early intervention. If you recognize any of these in yourself or a loved one, it's a signal to seek support. Managing stress is crucial for prevention and recovery. We offer resources on burnout and stress recovery.
Pathways to Wellness: Diagnosis and Evidence-Based Treatment
If you suspect you or a loved one is struggling with a perinatal mental health condition, know that effective diagnosis and treatment are available. Taking the first step is often the hardest, but it's the most crucial toward feeling better.
Getting a Diagnosis: Screening and Assessment
The path to diagnosis typically begins with an open conversation with a trusted healthcare provider. This could be your OB-GYN, primary care physician, or your baby's pediatrician. Pediatricians, in particular, are increasingly recognizing their vital role in screening for maternal mental health during routine well-child visits, framing it as a service to the child.
- Talking to a Healthcare Provider: Be honest and open about your feelings and symptoms. Your provider is there to help, not to judge.
- Screening Questionnaires: You may be asked to complete a screening tool, such as the Edinburgh Postnatal Depression Scale (EPDS). These questionnaires help identify potential symptoms and assess their severity.
- Importance of Honesty: It's essential to answer these questions as truthfully as possible, even if you feel ashamed or embarrassed. Seeking help is a sign of strength.
- What to Expect During an Assessment: A thorough assessment will involve discussing your symptoms, medical history, social support, and any risk factors. This helps your provider understand your unique situation and recommend the most appropriate course of action.
Leading organizations like the American College of Obstetricians and Gynecologists (ACOG) emphasize the importance of screening for perinatal mental health conditions. Their comprehensive toolkit provides guidance for healthcare professionals on detection, assessment, and treatment. You can find more information on ACOG's perinatal mental health programs.

Evidence-Based Therapy for Perinatal Mental Health
Once a diagnosis is made, several evidence-based therapeutic approaches have proven highly effective in treating PMADs. At Southlake Integrative Counseling and Wellness, we integrate these modalities into personalized treatment plans.
- Cognitive Behavioral Therapy (CBT): This widely recognized therapy helps individuals identify and change negative thought patterns and behaviors that contribute to their distress. It provides practical tools for managing anxiety, depression, and stress. Our practice specializes in Cognitive Behavioral Therapy to help you regain emotional balance.
- Interpersonal Therapy (IPT): IPT focuses on improving interpersonal relationships and social functioning, recognizing that difficulties in these areas can impact mood. It can be particularly helpful for new parents navigating relationship changes and social isolation.
- Accelerated Resolution Therapy (ART): ART is an innovative, evidence-based therapy that helps individuals process traumatic memories and difficult emotions quickly and effectively. This can be especially beneficial for those experiencing birth trauma or PTSD. Learn more about this powerful approach in our Complete Guide to Accelerated Resolution Therapy.
- Couples Counseling: PMADs can strain even the strongest relationships. Couples counseling can help partners communicate more effectively, steer challenges together, and rebuild intimacy and support.
- Group Therapy: Connecting with others who share similar experiences can be incredibly validating and empowering. Group therapy provides a safe space to share, learn, and receive support from peers.
We believe in a holistic approach to mental wellness, recognizing that mind and body are interconnected. Our approach integrates evidence-based therapies with alternative modalities to promote emotional balance and resilience. Explore how a holistic approach to therapy can support your healing journey.
Medication During and After Pregnancy: A Balanced View
For some individuals, medication can be a crucial component of their treatment plan, especially for moderate to severe PMADs. The decision to use medication during pregnancy or while breastfeeding is a highly personal one, made in careful consultation with your healthcare team.
- Antidepressants (SSRIs): Selective serotonin reuptake inhibitors (SSRIs) are often the first-line medication for perinatal depression and anxiety. Many are considered relatively safe during pregnancy and breastfeeding, with risks needing to be weighed against the risks of untreated maternal illness.
- Discussing Risks and Benefits with a Provider: It is essential to have an open and thorough discussion with your doctor about the potential risks and benefits of medication for both you and your baby. The risk of birth defects and other problems for babies of mothers who take antidepressants during pregnancy is very low. However, women should always let a health care provider know if they are pregnant or nursing and work with the provider to minimize the baby’s exposure to medication.
- Information on Medication Safety: Reliable resources like the FDA website provide comprehensive information on medication safety during pregnancy. You can also learn about specific medications and their latest approvals, side effects, and warnings on the FDA website for drugs.
- Newer Medications: The U.S. Food and Drug Administration (FDA) has approved specific medications like brexanolone and zuranolone for severe postpartum depression. Zuranolone offers an oral option, which can be more accessible for many.
- Making an Informed Decision: Your healthcare provider will help you weigh the potential benefits of improved maternal mental health against any potential risks to the baby. Untreated maternal depression and anxiety also carry significant risks for both mother and child, making treatment a vital consideration.
We encourage you to partner with your doctor to make an informed decision that prioritizes your well-being and the health of your family.
Building Your Support System: Resources and Community
Navigating perinatal mental health challenges is not something you should do alone. Building a strong support system of loved ones and professionals is essential for healing and recovery.
How Loved Ones Can Provide Meaningful Support
Family and friends play a critical role in supporting someone struggling with perinatal mental health issues. Often, they are the first to notice changes and can offer invaluable practical and emotional assistance.
- Offer Practical Help: New parents are often overwhelmed. Offer to help with chores, prepare meals, run errands, or take care of the baby so the parent can rest or attend appointments. "Can I bring you dinner?" or "Can I watch the baby for an hour while you nap?" are incredibly helpful questions.
- Listen Without Judgment: Sometimes, what's needed most is a non-judgmental ear. Listen to their feelings, fears, and frustrations without trying to "fix" everything. Validate their experience and remind them that their feelings are valid.
- Encourage Professional Help: Gently suggest seeking professional support. Offer to help them find a therapist, make appointments, or even accompany them to a session.
- Reassure Them They Are Not Alone: Remind them that many parents experience similar struggles, and it's not their fault. Reassure them that with help, they will feel better.
- Help Them Find Resources: Assist in researching local support groups, therapists, or online resources.
Developing healthy coping skills as a family unit can strengthen your resilience during this time. We offer resources to help you develop coping skills that benefit everyone.
Essential Resources for Diverse and Underserved Communities
It's crucial to acknowledge that perinatal mental health challenges can be compounded by unique stressors and systemic barriers for diverse populations, including Indigenous, LGBTQIA+, and racialized communities. Culturally safe care that understands and respects these experiences is paramount.
For instance, the Public Health Ontario webinar on 2SLGBTQIA+ Families – Unique Perinatal Mental Health Concerns highlights specific challenges faced by these families, such as discrimination, lack of affirming care, and unique family structures. Finding providers who are culturally competent and affirming can make a significant difference in access and effectiveness of care. We are committed to providing inclusive and personalized mental health care for all individuals in Southlake, TX.
Finding Professional and Peer Support
Fortunately, a wealth of resources exists to support individuals experiencing perinatal mental health challenges.
- National Hotlines:
- If you or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide & Crisis Lifeline at 988 or chat at 988lifeline.org. In life-threatening situations, always call 911.
- The National Maternal Mental Health Hotline (1-833-9-TLC-MAMA) offers free, confidential mental health support and resources.
- Postpartum Support International (PSI): PSI is a leading non-profit organization dedicated to helping those suffering from perinatal mood and anxiety disorders. They offer peer support groups, professional counseling, and extensive resources. You can visit their website at Postpartum Support International.
- Online and In-Person Support Groups: Connecting with others who understand can be incredibly healing. PSI offers online support groups, and many local communities also have in-person options.
- Finding a Certified Perinatal Mental Health Professional (PMH-C): For specialized care, look for a therapist with a PMH-C certification. This credential signifies specialized training and competency in perinatal mental health. Postpartum Support International (PSI) offers the world's first Certification in Perinatal Mental Health.
At Southlake Integrative Counseling and Wellness, we are dedicated to connecting you with the right support, whether it's within our practice or through trusted community partners.
Frequently Asked Questions about Perinatal Mental Health
We often hear similar questions from individuals and families navigating the complexities of the perinatal period. Here are some common inquiries and our expert answers.
Can partners and non-birthing parents experience perinatal mental health issues?
Absolutely, yes. While the focus often falls on birthing parents, partners and non-birthing parents are also susceptible to perinatal mental health challenges, often referred to as paternal perinatal depression or partner perinatal depression. Studies indicate that up to 10% of fathers can experience depression during the perinatal period.
Symptoms in partners might differ slightly from those in birthing parents and can include:
- Irritability, anger, or aggression
- Withdrawal from family life or social activities
- Increased stress, anxiety, or feelings of being overwhelmed
- Changes in sleep patterns or appetite
- Loss of interest in work or hobbies
- Physical symptoms like headaches or digestive issues
Support for the entire family unit is crucial, as a parent's mental health impacts everyone. We encourage partners to seek support if they are struggling, as their well-being is vital for the health of the whole family.
How long does it take to recover from a perinatal mood disorder?
Recovery from a perinatal mood disorder is highly individual and not always a linear process. It varies significantly based on several factors:
- Severity of the Condition: More severe disorders may require more intensive or longer-term treatment.
- Access to Treatment: Early intervention and consistent access to appropriate therapy and/or medication can significantly shorten the recovery timeline.
- Social Support: A strong network of family, friends, and community support can greatly aid recovery.
- Individual Resilience and Coping Skills: Everyone responds differently to treatment and life stressors.
With proper care, including evidence-based therapy and sometimes medication, significant improvement is expected. Many individuals begin to feel better within weeks or a few months of starting treatment, though full recovery may take longer. It's important to focus on progress, not perfection, and to be patient and compassionate with yourself throughout the journey. Seeking help is the most important step towards healing.
Are there holistic ways to support my mental health during this time?
Yes, absolutely! At Southlake Integrative Counseling and Wellness, we firmly believe in a holistic mental wellness approach that complements traditional therapies. Integrating mind-body practices can be incredibly effective in supporting your perinatal mental health journey.
Here are some holistic strategies we often recommend:
- Nutrition and Mood-Boosting Foods: What you eat can significantly impact your mood and energy levels. Focusing on a balanced diet rich in whole foods, omega-3 fatty acids, and probiotics can support brain health. Learn more about how food can positively influence your mood on our page about mood boosting foods.
- Gentle Exercise: Physical activity, even a short walk, can release endorphins and reduce stress. Listen to your body and engage in activities that feel good, like prenatal yoga, gentle stretching, or walking.
- Mindfulness and Meditation: Practicing mindfulness can help you stay present, manage anxiety, and develop a greater sense of calm. Simple breathing exercises or guided meditations can be integrated into your daily routine.
- Acupuncture: Some individuals find relief from anxiety and depression symptoms through acupuncture, an ancient healing practice.
- Mind-Body Massage Therapy: Massage can reduce stress hormones, improve circulation, and promote relaxation, fostering a deeper connection between your mind and body. Explore the benefits of mind-body massage therapy as a complementary treatment.
We incorporate these and other holistic coping strategies into our personalized treatment plans to support your overall well-being.
Conclusion: Nurturing Your Well-being on the Path to Parenthood
The journey through pregnancy and early parenthood is transformative, and it's entirely normal for it to come with its share of emotional ups and downs. However, if you find yourself experiencing persistent and overwhelming feelings of sadness, anxiety, or despair, it's crucial to remember: you are not alone. Perinatal mental health conditions are common, treatable, and seeking help is a profound sign of strength and a loving act toward yourself and your family.
At Southlake Integrative Counseling and Wellness, we are dedicated to supporting individuals and families in Southlake, TX, through every stage of this journey. We understand the unique challenges of the perinatal period and offer a compassionate, holistic approach to care. We integrate evidence-based therapies with mind-body practices to support your emotional well-being, helping you find balance, resilience, and joy in parenthood.
We invite you to reach out and explore how our comprehensive wellness services can support your healing journey. Your well-being matters, and we are here to help you thrive. Explore our comprehensive wellness services to start your healing journey.